LP(a) Cholesterol: It’s As Bad As They Say
By Dr. Norman E. Lepor
September 28, 2023
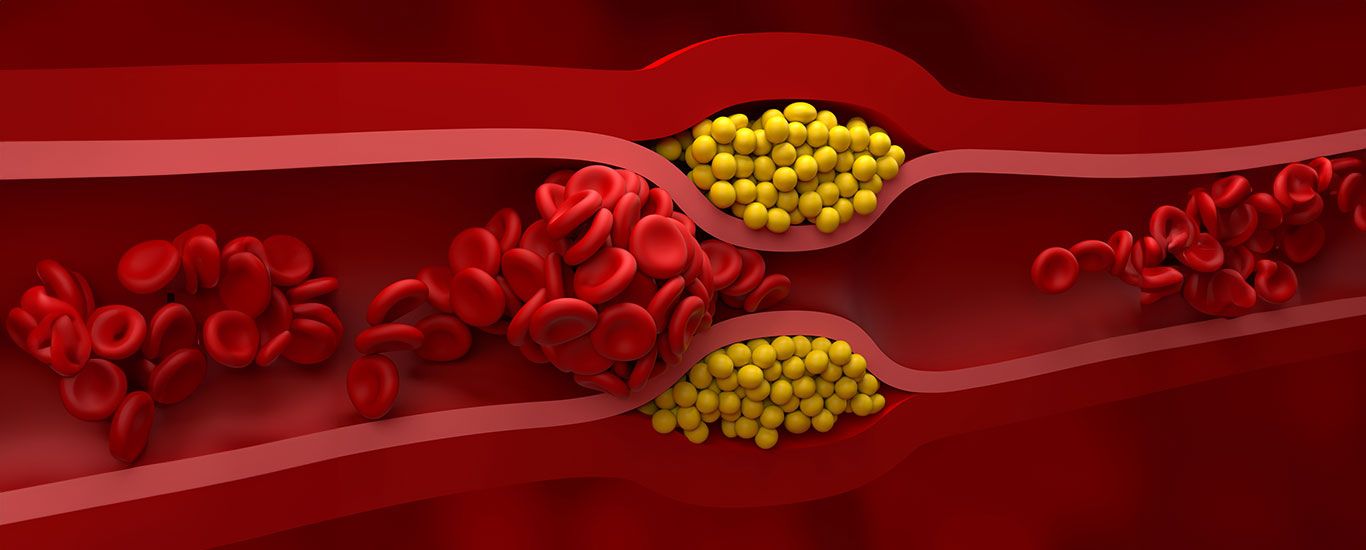
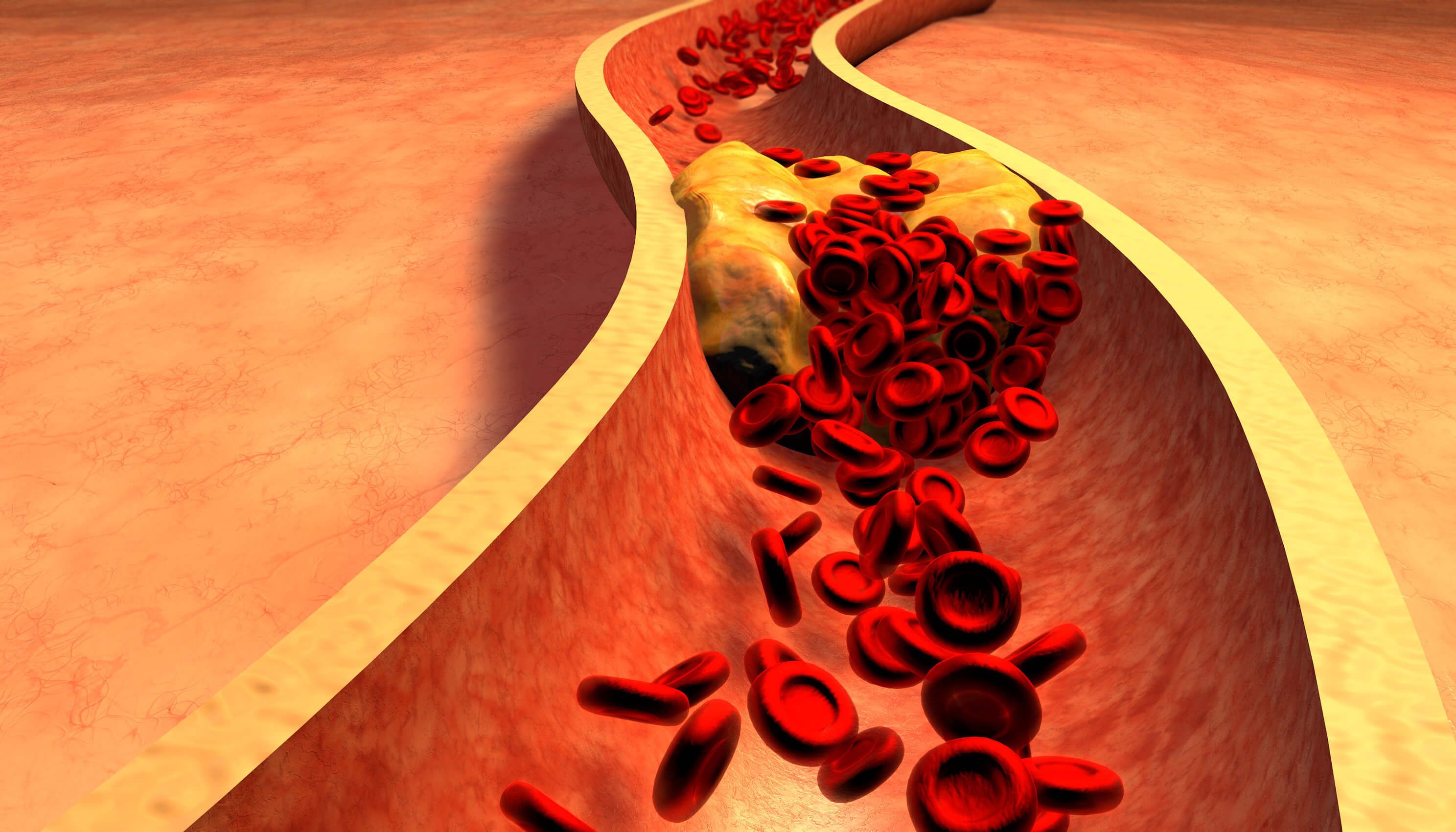
For the last forty years, the focus on reducing cardiovascular risk, meaning the risk of suffering a heart attack, stroke, amputation, or dying from these events, has been on lowering the bad cholesterol or LDL-cholesterol. In people who are considered high risk for suffering from heart and/or vascular disease, recommendations are for lowering LDL cholesterol to less than 50 mg/dl. But even in those who achieve this goal, many people have what is referred to as residual risk, meaning that their risk of suffering from complications of cardiovascular disease remains too high.
Lipoprotein A, also known by its abbreviation LP(a), was discovered only fifty years ago. It is associated with an increased risk of suffering from a heart attack, stroke, peripheral artery disease, and a valve condition called aortic stenosis independent of one’s cholesterol level. So even if your cholesterol is well treated, an elevated LP(a) can leave you at high risk.
How common is elevated Lp(a)?
It is estimated that up to 20% of people worldwide have high levels of LP(a), which is associated with a risk of heart attack or other serious cardiovascular events. A patient's LP(a) levels are one of the strongest indicators of their genetic risk for cardiovascular disease. People of African descent are found to have the highest concentration of Lp(a), while Chinese patients have the lowest LP(a) concentrations. Higher LP(a) concentrations were associated with an increased risk of heart attack in all ethnicities, particularly South Asians and Latin Americans. LP(a) is measured in two different units (mg/dl and nmol/l); therefore, it is really important to pay attention to the unit used for your test result. Normal LP(a) levels are less than 30 mg/dl or 75 nmol/l. An LP(a) level > 50 mg/dl or 100 nmol/l is associated with high cardiovascular risk.
Who should have their Lp(a) levels checked, and how often?
The newest recommendation is that LP(a) levels be checked once in all adults. People who have close relatives who have suffered from a heart attack, stroke, needed a stent or bypass surgery, or died at a younger age (under 65 years of age) from cardiovascular disease are more likely to have elevated LP(a) levels. Anyone with an elevated LP(a) level should also have their siblings and children checked, as they will have a 50% chance of having this problem.
LP(a) is not part of a routine cholesterol or lipid panel. You should ask your healthcare professional to check LP(a) levels. Since LP(a) levels are genetically determined, lifestyle modifications such as exercise and diet have little effect on LP(a). In fact, medications that are currently in use to lower LDL cholesterol have little effect on LP(a) levels and sometimes can actually increase levels.
What can I do if I have an elevated LP(a) level?
The good news is that there are now available, and only by participation in clinical trials, directed treatments for elevated LP(a). Since the liver cells make LP(a), these new treatments target the liver’s ability to make LP(a). These novel treatments can reduce LP(a) levels by as much as 90%.
Clinical trials are ongoing to evaluate the effect of treatments such as Olpasiran and Pelacarsen in Phase III clinical trials with other compounds such as SLN360 and LY3819469 in earlier clinical trial phases. These new treatments are given as easy-to-administer subcutaneous injections every one to three months, depending on the specific medication. It is hoped that by reducing LP(a) levels, one can reduce the risk of heart attack, stroke, and dying from cardiovascular disease.
Currently, the National Heart Institute is participating in the OCEAN(a) clinical trial, a Phase III trial evaluating the effect of Olpasiran in patients with a history of heart attack or coronary stent placement with an LP(a) level of 200 nmol/l or higher.
Why should I participate in a clinical trial?
Clinical trials are very important for patient care for a variety of reasons. Firstly, when you are involved in a clinical trial, we look at many contributing factors related to your specific condition and perform tests that may not be available through your health insurance or current healthcare provider. This way, we are able to get a very good assessment of your background and needs to determine which clinical trial may be best suited for you.
● NHI Clinical Trials are FREE
● No insurance is required
● You may be paid for participation
● Assistance with transportation may be provided
At NHI, we are committed to finding new and innovative treatment options for patients who suffer from cardiovascular and metabolic disorders.
To find out if you qualify, please fill out the NHI Candidate Form at https://nationalheartinstitute.org/candidate-form
For more information, get in touch with our NHI Research Team at info@nationalheartinstitute.org
We’re here to help!