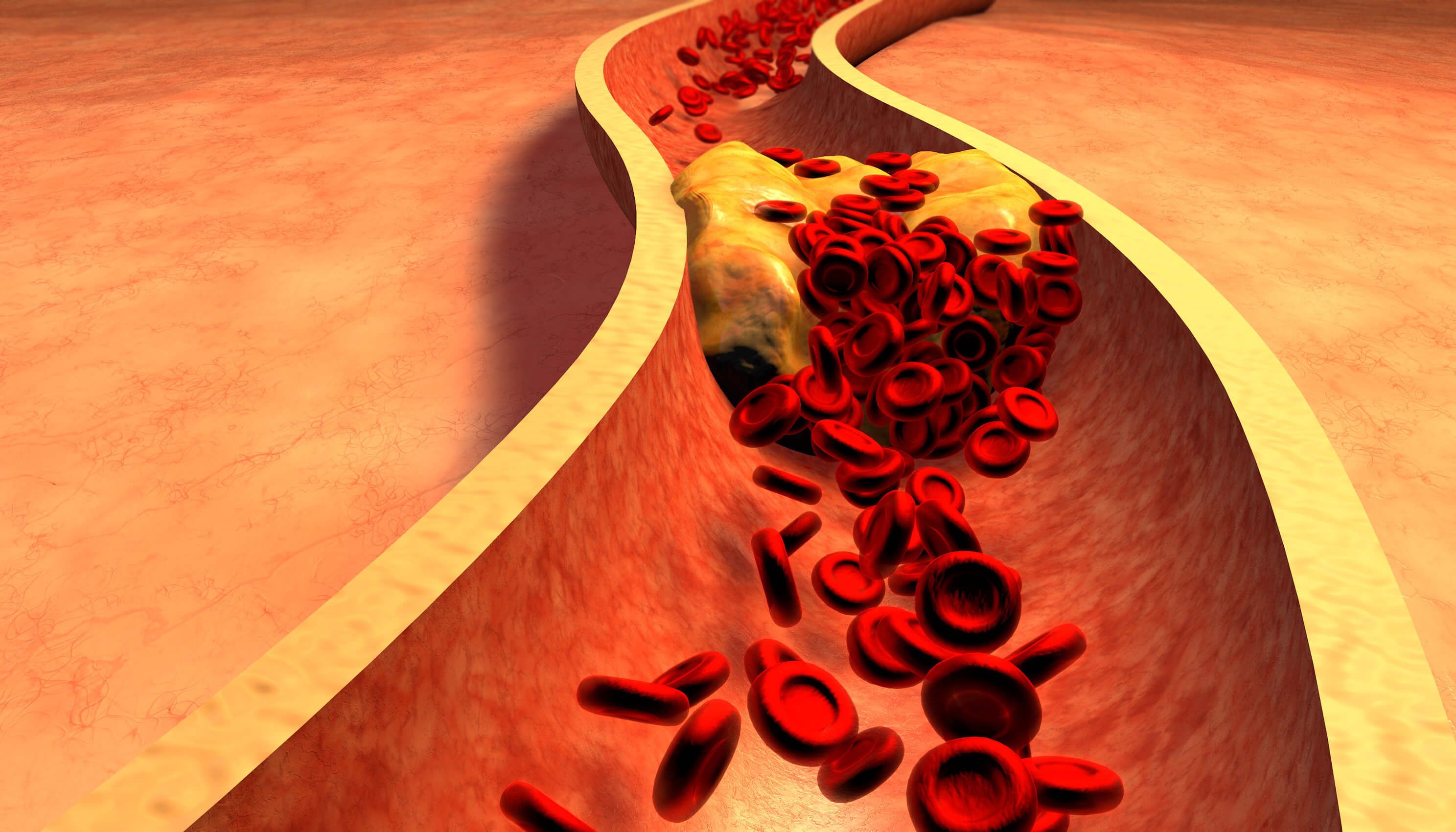
We know that LDL-cholesterol, otherwise known as the “bad cholesterol, plays a major role in the development of atherosclerosis or plaque formation in arteries. The most critical arteries include the coronary arteries to the heart, carotid arteries to the brain, and peripheral arteries to the legs, predisposing to sudden cardiac death, heart attack, stroke, and amputation. The higher the risk a person is for suffering from complications, the lower we want to get their cholesterol levels. If a patient has multiple risk factors, including elevated cholesterol or triglycerides, high blood pressure, diabetes, tobacco use, or a family history of coronary or vascular disease or has plaque seen on an imaging test such as a coronary calcium scan, coronary CT angiogram, or carotid artery ultrasound, we generally want the LDL-cholesterol levels to be near 70 mg/dl. If one has suffered from a cardiovascular event such as a heart attack, stroke, stent implant, or bypass surgery, we may want their LDL-cholesterols below 55 mg/dl, and in more severe cases, we may even want their LDL-cholesterol levels < 40 mg/dl. We have many treatments for LDL-cholesterol, including statins, bimedia acid, and PCSK9 regulating injectable medications.
But even if cholesterol is optimally treated, there remain other culprits that can lead to the progression of heart and vascular disease events. We call this “residual risk,” and contributors to this risk include lipoprotein (a), inflammation, and triglyceride-rich cholesterols. Measures of a test called NT-ProBNP can assess your cardiac stress level and predisposition to develop heart failure.
One should also know the level of a less known but much more malignant cholesterol called lipoprotein (a), often referred to as the “horrible cholesterol.” Lipoprotein (a) elevation is a genetic or inherited disorder that does not generally respond to conventional cholesterol-lowering medications, diet, or exercise. Elevated lipoprotein independently increases one’s risk of heart attack, stroke, and aortic stenosis. Recommendations are that everyone should have a lipoprotein (a) level checked once in their lifetime. Levels above 50 mg/dl or 125 nmol/l indicate a higher cardiovascular risk. If your levels are indicated, your close relatives should also be checked. The National Heart Institute is engaged in clinical trials with treatments that can reduce lipoprotein (a) by over 90%.
We now appreciate more than ever that inflammation plays an important role in the rusting of coronary, carotid arteries called atherosclerosis. We know that patients who suffer from excess inflammation, measured by a blood test called high sensitivity C-reactive protein (hsCRP) with a level > 2mg/L are at an increased risk of heart attack, stroke, peripheral artery disease, heart failure and kidney disease. We know that an anti-inflammatory drug that has been shown to reduce heart attack and stroke. The National Heart Institute is engaged in a clinical trial with a treatment that lowers the level of inflammation in patients with blockages in coronary, carotid, or peripheral arteries and or those patients with symptoms of heart failure such as shortness of breath, edema, and fatigue to determine if we can prevent heart attack, stroke, heart failure, and dialysis.
Triglycerides are a cholesterol precursor and part of a routine cholesterol blood test panel. Elevations of fasting triglyceride levels > 150 mg/dl are often ignored even though they are associated with “residual risk” of heart attack and stroke. People who are most likely to have elevated triglycerides are pre-diabetics and diabetics, obese, have low thyroid hormone levels, or consume alcohol. Often, elevated triglycerides are treated with medications that do NOT prevent heart attack and stroke, such as omega fish oils, niacin, or fenofibrates. The National Heart Institute is engaged in clinical trials of compounds that we hope will reduce high and very high triglycerides and also prevent heart attack, stroke, and pancreatitis.
NT-ProBNP is a blood test that is produced by the heart when it is under stress. It can identify patients who have heart failure or are at imminent risk of heart failure. It is an important test for your physician to consider performing if you feel fatigued or sort of breath or develop swelling in your ankles. The National Heart Institute is engaged in clinical trials to find better treatments to prevent and treat heart failure.
If you, a family member, or friend are considered to be at high risk of suffering from heart attack, stroke, sudden cardiac death, or heart failure because of diabetes, hypertension, tobacco use, a family history of cardiovascular disease, or have had an imaging test showing plaque or have suffered from a heart attack or stroke or had bypass surgery or a stent procedure, please check your lipoprotein (a) level, hs CRP, triglyceride and NT-ProBNP levels. The National Heart Institute is poised to be your partner to slash your “residual risk” through our elite clinical trial program.